Blood
For other uses, see Blood (disambiguation).
Blood is a bodily fluid in humans and other animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells.[1] When it reaches the lungs, gas exchange occurs when carbon dioxide is diffused out of the blood into thepulmonary alveoli and oxygen is diffused into the blood. This oxygenated blood is pumped to the left hand side of the heart in thepulmonary vein and enters the left atrium. From here it passes through the mitral valve, through the ventricle and taken all around the body by the aorta. Blood contains antibodies,nutrients, oxygen and much more to help the body work.[citation needed]
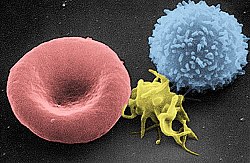
In vertebrates, it is composed of blood cellssuspended in blood plasma. Plasma, which constitutes 55% of blood fluid, is mostly water (92% by volume),[2] and contains dissipatedproteins, glucose, mineral ions, hormones, carbon dioxide (plasma being the main medium for excretory product transportation), and blood cells themselves. Albumin is the main protein in plasma, and it functions to regulate the colloidal osmotic pressure of blood. The blood cells are mainly red blood cells (also called RBCs or erythrocytes), white blood cells (also called WBCs or leukocytes) and platelets. The most abundant cells in vertebrate blood are red blood cells. These contain hemoglobin, an iron-containing protein, which facilitates oxygen transport by reversibly binding to this respiratory gas and greatly increasing its solubility in blood. In contrast, carbon dioxide is almost entirely transported extracellularly dissolved in plasma as bicarbonate ion.[citation needed]
Vertebrate blood is bright red when its haemoglobin is oxygenated and dark red when it is deoxygenated. Some animals, such as crustaceans and mollusks, usehemocyanin to carry oxygen, instead of hemoglobin. Insects and some mollusks use a fluid called hemolymph instead of blood, the difference being that hemolymph is not contained in a closed circulatory system. In most insects, this "blood" does not contain oxygen-carrying molecules such as hemoglobin because their bodies are small enough for their tracheal system to suffice for supplying oxygen.
Jawed vertebrates have an adaptive immune system, based largely on white blood cells. White blood cells help to resist infections and parasites. Platelets are important in theclotting of blood. Arthropods, using hemolymph, have hemocytes as part of theirimmune system.
Blood is circulated around the body throughblood vessels by the pumping action of theheart. In animals with lungs, arterial blood carries oxygen from inhaled air to the tissues of the body, and venous blood carries carbon dioxide, a waste product of metabolismproduced by cells, from the tissues to the lungs to be exhaled.
Medical terms related to blood often begin with hemo- or hemato- (also spelled haemo-and haemato-) from the Greek word αἷμα(haima) for "blood". In terms of anatomy andhistology, blood is considered a specialized form of connective tissue, given its origin in the bones and the presence of potential molecular fibers in the form of fibrinogen.
Functions
Blood performs many important functions within the body including:
- Supply of oxygen to tissues (bound tohemoglobin, which is carried in red cells)
- Supply of nutrients such as glucose, amino acids, and fatty acids (dissolved in the blood or bound to plasma proteins (e.g., blood lipids))
- Removal of waste such as carbon dioxide,urea, and lactic acid
- Immunological functions, including circulation of white blood cells, and detection of foreign material by antibodies
- Coagulation, the response to a broken blood vessel, the conversion of blood from a liquid to a semi-solid gel to stop bleeding.
- Messenger functions, including the transport of hormones and the signaling oftissue damage
- Regulation of body pH
- Regulation of core body temperature
- Hydraulic functions
Constituents
See also: Reference ranges for common blood tests
What's Inside of Blood
Blood accounts for 7% of the human body weight,[3][4] with an average density of approximately 1060 kg/m3, very close to pure water's density of 1000 kg/m3.[5] The average adult has a blood volume of roughly 5 litres(11 US pt),[4] which is composed of plasma and several kinds of cells. These blood cells (which are also called corpuscles or "formed elements") consist of erythrocytes (red blood cells, RBCs), leukocytes (white blood cells), and thrombocytes (platelets). By volume, the red blood cells constitute about 45% of whole blood, the plasma about 54.3%, and white cells about 0.7%.
Whole blood (plasma and cells) exhibits non-Newtonian fluid dynamics. If all human hemoglobin were free in the plasma rather than being contained in RBCs, the circulatory fluid would be too viscous for the cardiovascular system to function effectively.
Cells
Further information: Complete blood count
One microliter of blood contains:
- 4.7 to 6.1 million (male), 4.2 to 5.4 million (female) erythrocytes:[6] Red blood cells contain the blood's hemoglobin and distribute oxygen. Mature red blood cells lack a nucleusand organelles in mammals. The red blood cells (together with endothelial vessel cells and other cells) are also marked byglycoproteins that define the different blood types. The proportion of blood occupied by red blood cells is referred to as thehematocrit, and is normally about 45%. The combined surface area of all red blood cells of the human body would be roughly 2,000 times as great as the body's exterior surface.[7]
- 4,000–11,000 leukocytes:[8] White blood cells are part of the body's immune system; they destroy and remove old or aberrant cells and cellular debris, as well as attack infectious agents (pathogens) and foreign substances. The cancer of leukocytes is called leukemia.
- 200,000–500,000 thrombocytes:[8] Also called platelets, they take part in blood clotting (coagulation). Fibrin from the coagulation cascade creates a mesh over the platelet plug.
Plasma
Main article: Blood plasma
About 55% of blood is blood plasma, a fluid that is the blood's liquid medium, which by itself is straw-yellow in color. The blood plasma volume totals of 2.7–3.0 liters (2.8–3.2 quarts) in an average human. It is essentially an aqueous solution containing 92% water, 8% blood plasma proteins, and trace amounts of other materials. Plasma circulates dissolved nutrients, such asglucose, amino acids, and fatty acids(dissolved in the blood or bound to plasma proteins), and removes waste products, such as carbon dioxide, urea, and lactic acid.
Other important components include:
- Serum albumin
- Blood-clotting factors (to facilitatecoagulation)
- Immunoglobulins (antibodies)
- lipoprotein particles
- Various other proteins
- Various electrolytes (mainly sodium andchloride)
The term serum refers to plasma from which the clotting proteins have been removed. Most of the proteins remaining are albumin and immunoglobulins.
pH values
See also: Acid-base homeostasis
Blood pH is regulated to stay within the narrow range of 7.35 to 7.45, making it slightly basic.[9][10] Blood that has a pH below 7.35 is too acidic, whereas blood pH above 7.45 is too basic. Blood pH, partial pressureof oxygen (pO2), partial pressure of carbon dioxide (pCO2), and HCO3− are carefully regulated by a number of homeostatic mechanisms, which exert their influence principally through the respiratory systemand the urinary system in order to control theacid-base balance and respiration. An arterial blood gas test will measure these. Plasma also circulates hormones transmitting their messages to various tissues. The list of normal reference ranges for various blood electrolytes is extensive.
Blood in non-mammalian vertebrates
Human blood is typical of that of mammals, although the precise details concerning cell numbers, size, protein structure, and so on, vary somewhat between species. In non-mammalian vertebrates, however, there are some key differences:[11]
- Red blood cells of non-mammalian vertebrates are flattened and ovoid in form, and retain their cell nuclei
- There is considerable variation in the types and proportions of white blood cells; for example, acidophils are generally more common than in humans
- Platelets are unique to mammals; in other vertebrates, small nucleated, spindle cells called thrombocytes are responsible for blood clotting instead
Physiology
Cardiovascular system
Main article: Circulatory system
Blood is circulated around the body throughblood vessels by the pumping action of theheart. In humans, blood is pumped from the strong left ventricle of the heart througharteries to peripheral tissues and returns to the right atrium of the heart through veins. It then enters the right ventricle and is pumped through the pulmonary artery to the lungs and returns to the left atrium through thepulmonary veins. Blood then enters the left ventricle to be circulated again. Arterial blood carries oxygen from inhaled air to all of the cells of the body, and venous blood carries carbon dioxide, a waste product ofmetabolism by cells, to the lungs to be exhaled. However, one exception includes pulmonary arteries, which contain the most deoxygenated blood in the body, while the pulmonary veins contain oxygenated blood.
Additional return flow may be generated by the movement of skeletal muscles, which can compress veins and push blood through the valves in veins toward the right atrium.
The blood circulation was famously described by William Harvey in 1628.[12]
Production and degradation of blood cells
In vertebrates, the various cells of blood are made in the bone marrow in a process calledhematopoiesis, which includeserythropoiesis, the production of red blood cells; and myelopoiesis, the production of white blood cells and platelets. During childhood, almost every human bone produces red blood cells; as adults, red blood cell production is limited to the larger bones: the bodies of the vertebrae, the breastbone (sternum), the ribcage, the pelvic bones, and the bones of the upper arms and legs. In addition, during childhood, the thymus gland, found in the mediastinum, is an important source of T lymphocytes.[13] The proteinaceous component of blood (including clotting proteins) is produced predominantly by the liver, while hormones are produced by the endocrine glands and the watery fraction is regulated by the hypothalamus and maintained by the kidney.
Healthy erythrocytes have a plasma life of about 120 days before they are degraded by the spleen, and the Kupffer cells in the liver. The liver also clears some proteins, lipids, and amino acids. The kidney actively secretes waste products into the urine.
Oxygen transport
About 98.5% of the oxygen in a sample of arterial blood in a healthy human breathing air at sea-level pressure is chemically combined with the Hgb. About 1.5% is physically dissolved in the other blood liquids and not connected to Hgb. The hemoglobinmolecule is the primary transporter of oxygen in mammals and many other species (for exceptions, see below). Hemoglobin has an oxygen binding capacity of between 1.36 and 1.37 ml O2 per gram hemoglobin,[14] which increases the total blood oxygen capacityseventyfold,[15] compared to if oxygen solely were carried by its solubility of 0.03 ml O2 per liter blood per mm Hg partial pressure of oxygen (approximately 100 mm Hg in arteries).[15]
With the exception of pulmonary andumbilical arteries and their corresponding veins, arteries carry oxygenated blood away from the heart and deliver it to the body viaarterioles and capillaries, where the oxygen is consumed; afterwards, venules, and veins carry deoxygenated blood back to the heart.
Under normal conditions in adult humans at rest; hemoglobin in blood leaving the lungs is about 98–99% saturated with oxygen, achieving an oxygen delivery of between 950 and 1150 ml/min[16] to the body. In a healthy adult at rest, oxygen consumption is approximately 200 - 250 ml/min,[16] anddeoxygenated blood returning to the lungs is still approximately 75%[17][18] (70 to 78%)[16]saturated. Increased oxygen consumption during sustained exercise reduces the oxygen saturation of venous blood, which can reach less than 15% in a trained athlete; although breathing rate and blood flow increase to compensate, oxygen saturation in arterial blood can drop to 95% or less under these conditions.[19] Oxygen saturation this low is considered dangerous in an individual at rest (for instance, during surgery under anesthesia). Sustained hypoxia (oxygenation of less than 90%), is dangerous to health, and severe hypoxia (saturations of less than 30%) may be rapidly fatal.[20]
A fetus, receiving oxygen via the placenta, is exposed to much lower oxygen pressures (about 21% of the level found in an adult's lungs), and, so, fetuses produce another form of hemoglobin with a much higher affinity for oxygen (hemoglobin F) in order to function under these conditions.[21]
Carbon dioxide transport
CO2 is carried in blood in three different ways. (The exact percentages vary depending whether it is arterial or venous blood). Most of it (about 70%) is converted to bicarbonate ions HCO−
3 by the enzyme carbonic anhydrase in the red blood cells by the reaction CO2 + H2O → H2CO3 → H+ + HCO−
3; about 7% is dissolved in the plasma; and about 23% is bound to hemoglobin ascarbamino compounds.[22] Hemoglobin, the main oxygen-carrying molecule in red blood cells, carries both oxygen and carbon dioxide. However, the CO2 bound to hemoglobin does not bind to the same site as oxygen. Instead, it combines with the N-terminal groups on the four globin chains. However, because ofallosteric effects on the hemoglobin molecule, the binding of CO2 decreases the amount of oxygen that is bound for a given partial pressure of oxygen. The decreased binding to carbon dioxide in the blood due to increased oxygen levels is known as theHaldane effect, and is important in the transport of carbon dioxide from the tissues to the lungs. A rise in the partial pressure of CO2 or a lower pH will cause offloading of oxygen from hemoglobin, which is known as the Bohr effect.
3 by the enzyme carbonic anhydrase in the red blood cells by the reaction CO2 + H2O → H2CO3 → H+ + HCO−
3; about 7% is dissolved in the plasma; and about 23% is bound to hemoglobin ascarbamino compounds.[22] Hemoglobin, the main oxygen-carrying molecule in red blood cells, carries both oxygen and carbon dioxide. However, the CO2 bound to hemoglobin does not bind to the same site as oxygen. Instead, it combines with the N-terminal groups on the four globin chains. However, because ofallosteric effects on the hemoglobin molecule, the binding of CO2 decreases the amount of oxygen that is bound for a given partial pressure of oxygen. The decreased binding to carbon dioxide in the blood due to increased oxygen levels is known as theHaldane effect, and is important in the transport of carbon dioxide from the tissues to the lungs. A rise in the partial pressure of CO2 or a lower pH will cause offloading of oxygen from hemoglobin, which is known as the Bohr effect.
Transport of hydrogen ions
Some oxyhemoglobin loses oxygen and becomes deoxyhemoglobin. Deoxyhemoglobin binds most of the hydrogen ions as it has a much greater affinity for more hydrogen than does oxyhemoglobin.
Lymphatic system
Main article: Lymphatic system
In mammals, blood is in equilibrium withlymph, which is continuously formed in tissues from blood by capillary ultrafiltration. Lymph is collected by a system of small lymphatic vessels and directed to thethoracic duct, which drains into the leftsubclavian vein where lymph rejoins the systemic blood circulation.
Thermoregulation
Blood circulation transports heat throughout the body, and adjustments to this flow are an important part of thermoregulation. Increasing blood flow to the surface (e.g., during warm weather or strenuous exercise) causes warmer skin, resulting in faster heat loss. In contrast, when the external temperature is low, blood flow to the extremities and surface of the skin is reduced and to prevent heat loss and is circulated to the important organs of the body, preferentially.
Hydraulic functions
The restriction of blood flow can also be used in specialized tissues to cause engorgement, resulting in an erection of that tissue; examples are the erectile tissue in the penisand clitoris.
Another example of a hydraulic function is the jumping spider, in which blood forced into the legs under pressure causes them to straighten for a powerful jump, without the need for bulky muscular legs.[23]
Invertebrates
In insects, the blood (more properly calledhemolymph) is not involved in the transport of oxygen. (Openings called tracheae allow oxygen from the air to diffuse directly to the tissues). Insect blood moves nutrients to the tissues and removes waste products in an open system.
Other invertebrates use respiratory proteins to increase the oxygen-carrying capacity. Hemoglobin is the most common respiratory protein found in nature. Hemocyanin (blue) contains copper and is found in crustaceansand mollusks. It is thought that tunicates (sea squirts) might use vanabins (proteins containing vanadium) for respiratory pigment(bright-green, blue, or orange).
In many invertebrates, these oxygen-carrying proteins are freely soluble in the blood; in vertebrates they are contained in specialized red blood cells, allowing for a higher concentration of respiratory pigments without increasing viscosity or damaging blood filtering organs like the kidneys.
Giant tube worms have unusual hemoglobins that allow them to live in extraordinary environments. These hemoglobins also carry sulfides normally fatal in other animals.
Color
The coloring matter of blood (hemochrome) is largely due to the protein in the blood responsible for oxygen transport. Different groups of organisms use different proteins.
Hemoglobin
Main article: Hemoglobin
Hemoglobin is the principal determinant of the color of blood in vertebrates. Each molecule has four heme groups, and their interaction with various molecules alters the exact color. In vertebrates and other hemoglobin-using creatures, arterial blood and capillary blood are bright red, as oxygen imparts a strong red color to the heme group. Deoxygenated blood is a darker shade of red; this is present in veins, and can be seen during blood donation and when venous blood samples are taken. This is because the spectrum of light absorbed by hemoglobin differs between the oxygenated and deoxygenated states.[24]
Blood in carbon monoxide poisoning is bright red, because carbon monoxide causes the formation of carboxyhemoglobin. In cyanidepoisoning, the body cannot utilize oxygen, so the venous blood remains oxygenated, increasing the redness. There are some conditions affecting the heme groups present in hemoglobin that can make the skin appear blue—a symptom called cyanosis. If the heme is oxidized, methaemoglobin, which is more brownish and cannot transport oxygen, is formed. In the rare conditionsulfhemoglobinemia, arterial hemoglobin is partially oxygenated, and appears dark red with a bluish hue.
Veins close to the surface of the skin appear blue for a variety of reasons. However, the factors that contribute to this alteration ofcolor perception are related to the light-scattering properties of the skin and the processing of visual input by the visual cortex, rather than the actual color of the venous blood.[25]
Skinks in the genus Prasinohaema have green blood due to a buildup of the waste productbiliverdin.[26]
Hemocyanin
Main article: Hemocyanin
The blood of most mollusks – includingcephalopods and gastropods – as well as some arthropods, such as horseshoe crabs, is blue, as it contains the copper-containing protein hemocyanin at concentrations of about 50 grams per liter.[27] Hemocyanin is colorless when deoxygenated and dark blue when oxygenated. The blood in the circulation of these creatures, which generally live in cold environments with low oxygen tensions, is grey-white to pale yellow,[27] and it turns dark blue when exposed to the oxygen in the air, as seen when they bleed.[27] This is due to change in color of hemocyanin when it is oxidized.[27] Hemocyanin carries oxygen inextracellular fluid, which is in contrast to the intracellular oxygen transport in mammals by hemoglobin in RBCs.[27]
Chlorocruorin
Main article: Chlorocruorin
The blood of most annelid worms and some marine polychaetes use chlorocruorin to transport oxygen. It is green in color in dilute solutions.[28]
Hemerythrin
Main article: Hemerythrin
Hemerythrin is used for oxygen transport in the marine invertebrates sipunculids,priapulids, brachiopods, and the annelid worm, magelona. Hemerythrin is violet-pink when oxygenated.[28]
Hemovanadin
Main article: Hemovanadin
The blood of some species of ascidians and tunicates, also known as sea squirts, contains proteins called vanabins. These proteins are based on vanadium, and give the creatures a concentration of vanadium in their bodies 100 times higher than the surrounding sea water. Unlike hemocyanin and hemoglobin, hemovanadin is not an oxygen carrier. When exposed to oxygen, however, vanabins turn a mustard yellow.
Pathology
General medical disorders
- Disorders of volume
- Injury can cause blood loss through bleeding.[29] A healthy adult can lose almost 20% of blood volume (1 L) before the first symptom, restlessness, begins, and 40% of volume (2 L) before shock sets in. Thrombocytes are important for bloodcoagulation and the formation of blood clots, which can stop bleeding. Trauma to the internal organs or bones can causeinternal bleeding, which can sometimes be severe.
- Dehydration can reduce the blood volume by reducing the water content of the blood. This would rarely result in shock(apart from the very severe cases) but may result in orthostatic hypotension andfainting.
- Disorders of circulation
- Shock is the ineffective perfusion of tissues, and can be caused by a variety of conditions including blood loss, infection, poor cardiac output.
- Atherosclerosis reduces the flow of blood through arteries, because atheroma lines arteries and narrows them. Atheroma tends to increase with age, and its progression can be compounded by many causes including smoking, high blood pressure, excess circulating lipids (hyperlipidemia), and diabetes mellitus.
- Coagulation can form a thrombosis, which can obstruct vessels.
- Problems with blood composition, the pumping action of the heart, or narrowing of blood vessels can have many consequences including hypoxia (lack of oxygen) of the tissues supplied. The termischemia refers to tissue that is inadequately perfused with blood, andinfarction refers to tissue death (necrosis), which can occur when the blood supply has been blocked (or is very inadequate)
Hematological disorders
See also: Hematology
- Anemia
- Insufficient red cell mass (anemia) can be the result of bleeding, blood disorders like thalassemia, or nutritional deficiencies; and may require blood transfusion. Several countries have blood banks to fill the demand for transfusable blood. A person receiving a blood transfusion must have ablood type compatible with that of the donor.
- Sickle-cell anemia
- Disorders of cell proliferation
- Leukemia is a group of cancers of the blood-forming tissues and cells.
- Non-cancerous overproduction of red cells (polycythemia vera) or platelets (essential thrombocytosis) may bepremalignant.
- Myelodysplastic syndromes involve ineffective production of one or more cell lines.
- Disorders of coagulation
- Hemophilia is a genetic illness that causes dysfunction in one of the blood'sclotting mechanisms. This can allow otherwise inconsequential wounds to be life-threatening, but more commonly results in hemarthrosis, or bleeding into joint spaces, which can be crippling.
- Ineffective or insufficient platelets can also result in coagulopathy (bleeding disorders).
- Hypercoagulable state (thrombophilia) results from defects in regulation of platelet or clotting factor function, and can cause thrombosis.
- Infectious disorders of blood
- Blood is an important vector of infection. HIV, the virus that causes AIDS, is transmitted through contact with blood, semen or other body secretions of an infected person. Hepatitis B and C are transmitted primarily through blood contact. Owing to blood-borne infections, bloodstained objects are treated as abiohazard.
- Bacterial infection of the blood isbacteremia or sepsis. Viral Infection is viremia. Malaria and trypanosomiasis are blood-borne parasitic infections.
Carbon monoxide poisoning
Main article: Carbon monoxide poisoning
Substances other than oxygen can bind to hemoglobin; in some cases this can cause irreversible damage to the body. Carbon monoxide, for example, is extremely dangerous when carried to the blood via the lungs by inhalation, because carbon monoxide irreversibly binds to hemoglobin to form carboxyhemoglobin, so that less hemoglobin is free to bind oxygen, and fewer oxygen molecules can be transported throughout the blood. This can cause suffocation insidiously. A fire burning in an enclosed room with poor ventilation presents a very dangerous hazard, since it can create a build-up of carbon monoxide in the air. Some carbon monoxide binds to hemoglobin when smoking tobacco.[citation needed]
Medical treatments
Blood products
Further information: Blood transfusion
Blood for transfusion is obtained from human donors by blood donation and stored in ablood bank. There are many different blood types in humans, the ABO blood group system, and the Rhesus blood group systembeing the most important. Transfusion of blood of an incompatible blood group may cause severe, often fatal, complications, socrossmatching is done to ensure that a compatible blood product is transfused.
Other blood products administeredintravenously are platelets, blood plasma, cryoprecipitate, and specific coagulation factor concentrates.
Intravenous administration
Many forms of medication (from antibioticsto chemotherapy) are administered intravenously, as they are not readily or adequately absorbed by the digestive tract.
After severe acute blood loss, liquid preparations, generically known as plasma expanders, can be given intravenously, either solutions of salts (NaCl, KCl, CaCl2 etc.) at physiological concentrations, or colloidal solutions, such as dextrans, human serum albumin, or fresh frozen plasma. In these emergency situations, a plasma expander is a more effective life-saving procedure than a blood transfusion, because the metabolism of transfused red blood cells does not restart immediately after a transfusion.
Bloodletting
Main article: bloodletting
In modern evidence-based medicine, bloodletting is used in management of a few rare diseases, including hemochromatosisand polycythemia. However, bloodletting andleeching were common unvalidated interventions used until the 19th century, as many diseases were incorrectly thought to be due to an excess of blood, according toHippocratic medicine.
















No comments:
Post a Comment